More than 2 million Americans live with limb loss, a testament to the scale of this medical and social issue. Our coverage takes a look at these numbers, examining the prevalence, causes, and impacts of amputation on individuals and healthcare systems.
Key Takeaways
- Over 2 million Americans are living with limb loss, with vascular diseases (54%) and trauma (45%) being the leading causes of amputations.
- Diabetes and peripheral arterial disease (PAD) play prominent roles in lower extremity amputations, and the economic impact of diabetes-related amputations on US healthcare exceeds $4.3 billion annually.
- Technological advancements in prosthetics are enhancing the quality of life for amputees, with AI and machine learning contributing to more intuitive and adaptive control.
Current Statistics on Amputees in the United States
Given a population exceeding 330 million, the fact that over 2 million Americans live with limb loss is indeed striking. This number has been steadily increasing over the years, with around 185,000 amputations occurring annually. But what’s behind these numbers?
The causes of limb loss in the United States are diverse. The majority, about 54%, are due to vascular diseases, followed by trauma at 45%, and a small fraction, less than 2%, are due to cancer. These numbers reflect the significant role of chronic health conditions and accidents in the prevalence of limb loss.
Causes Behind Lower Extremity Amputations

While several conditions can lead to lower limb amputations, certain diseases are particularly notorious. Dysvascular diseases, such as peripheral vascular disease and diabetes, are the leading causes of lower extremity amputations, accounting for up to a staggering 93.4% of cases.
With its increasing public health prominence, diabetes mellitus presents significant risks for complications in the lower extremities. Up to one-quarter of diabetic patients develop foot ulcers, which can ultimately lead to amputation. These foot ulcers can get complicated by infection, osteomyelitis, and gangrene, dramatically increasing the likelihood of requiring an amputation. The economic burden of these diabetes-related lower extremity amputations on the United States healthcare system exceeds $4.3 billion annually.
The Impact of Vascular Disease on Limb Loss
Focusing on the vascular diseases contributing significantly to amputation statistics, peripheral arterial disease (PAD) accounts for more than 150,000 foot amputations each year in the U.S., affecting toes, legs, or feet. The mortality rates associated with PAD are startlingly high. Nearly half of those with an amputation due to vascular disease will die within five years, surpassing five-year mortality rates for many cancers.
Risk factors for PAD include hypertension, diabetes, smoking, high cholesterol, obesity, lack of exercise, and genetic predisposition.
Traumatic Amputations: Prevalence and Prevention
In addition to diseases, accidents or trauma-related injuries can also result in amputations. High-energy traumatic injuries are a significant cause of amputations, with over 20% leading to amputation when associated with severe wound contamination and significant soft tissue loss.
The leading cause of traumatic amputations worldwide is:
- Falls, accounting for about 36% of cases
- Road injuries, accounting for about 15% of cases
- Other transportation injuries, accounting for about 11% of cases
- Mechanical forces, accounting for about 10% of cases
These statistics underscore the importance of implementing safety protocols, preventive interventions, and methods to treat traumatic amputations in order to decrease the occurrence of prevalent traumatic amputations.
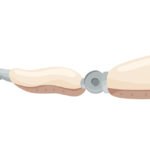
Technological Advances in Prosthetic Devices

Despite the sobering statistics, amputees today can find hope in the rapidly advancing prosthetic device technology. These devices now utilize technologies like target muscle reinnervation, regenerative peripheral nerve interfaces, and osseointegrated prostheses.
Artificial intelligence and machine learning enable prosthetic hands to adjust grip autonomously and bionic legs to adapt to varied terrains. Alongside this, AI-based systems interpret nerve interface signals for intuitive prosthetic control. These technological advancements play a pivotal role in the rehabilitation of amputees, significantly contributing to their quality of life and successful reintegration into daily life.
Living with Limb Loss: Challenges and Support Systems

The challenges of living with limb loss extend beyond physical implications, encompassing emotional and psychological elements as well. Some of the emotional reactions that amputees often undergo include:
- Grief
- Anxiety
- Depression
- Altering self-esteem
- Body image perceptions
Depression can occur in about 20% to 60% of amputees, and anxiety in 25% to 57% – rates substantially higher than in the general population.
Amputees employ various coping styles, ranging from adaptive tactics such as humor and active problem-solving to maladaptive behaviors including avoidance and overcompensation. Some even report positive outcomes post-amputation, citing greater independence, better coping skills, and a transformed attitude towards life.
The support system for amputees plays a crucial role in successful adaptation to limb loss. Social support, including from family, friends, and peer groups, is essential. Amputee education groups and spiritual services play significant roles in extended support and community reintegration.
The Economics of Amputation: Healthcare Costs and Prosthetic Services
Amputations carry not just emotional and physical burdens, but also bear a significant economic impact. Hospital costs associated with amputation amounted to over $8.3 billion in 2009, with diabetic patients facing increased financial burdens as their lifetime healthcare costs due to amputation surpass $4.3 billion annually in the USA.
Policy advancements are continually being made to address these economic challenges. However, significant challenges lie in making advanced prosthetics cost-effective and widely accessible, necessitating collaborations between engineers and health agencies.
Demographics: A Closer Look at Who is Affected
Demographic factors exert influence on both the prevalence and risk of amputation. African-Americans are up to four times more likely to have an amputation than white Americans, with similar increased risks observed in African American, Hispanic, and American Indian individuals with diabetic foot ulcers (DFUs) compared to their white counterparts.
As far as age and gender are concerned:
- Males are twice as likely to undergo limb amputation than females.
- The rate of limb amputation increases with age.
- Individuals over 50 experience the highest increase in limb amputation over a 14-year period.
Regional Variations in Amputation Rates
Amputation rates vary regionally, reflecting influences from local healthcare systems, socioeconomic status, and disease prevalence. In developed countries such as the United States, Denmark, and Japan, 68% of all amputations are due to diseases like diabetes and peripheral vascular disease.
Conversely, in developing countries, trauma from accidents and inadequately treated injuries is the leading cause of amputation. Such variations underscore the need for policies and interventions tailored to specific regional contexts and demographics.
Rehabilitation and Recovery Post-Amputation
Post-amputation recovery is a complex journey necessitating an interprofessional team. This team includes:
- a physical medicine and rehabilitation doctor
- nursing staff
- pharmacists
- occupational therapists
- prosthetists
- psychologists
- multispecialty physicians
Physical and emotional recovery is integral to rehabilitation. While aging can affect the fitting of prostheses and rehabilitation outcomes, older adults, even those over 80, can successfully use a prosthesis and achieve substantial independence. Emotional recovery addresses grief and potential mental health issues, including post-traumatic stress disorder (PTSD).
Functional assessment for lower limb amputees, following a lower limb amputation, is conducted by a team approach. The choice of whether to use a prosthetic device is influenced by various factors such as the extremity amputated, age, and general health. Clear communication with the patient about treatment and expectations is crucial pre-operatively, and face-to-face communication during patient hand-off ensures continuity of care post-surgery.
Raising Awareness and Advocacy Efforts
Support for the amputee community hinges on the vital tasks of raising awareness and advocacy. The Amputee Coalition organizes Limb Loss and Limb Difference Awareness Month, which includes various online tools and social activities to increase engagement and awareness. The Amputee Coalition National Conference serves as an educational platform and networking event, unifying voices on critical issues.
These efforts, alongside research and data collection, inform policy and improve the allocation of support services for disease control, advocating for better outcomes for the community.
Innovations in Pain Control and Phantom Limb Management
Following amputation, many amputees encounter a phenomenon termed phantom limb pain (PLP) not only in the amputated limb but also occasionally in the contralateral limb. Approximately 60% to 80% of amputees develop PLP, which involves complex etiological factors including cortical reorganization and peripheral-nerve hyperexcitability.
The management of PLP includes a variety of pharmacologic treatments such as:
- Anticonvulsants
- Antidepressants
- Opioids
- Anesthetics
- NMDA receptor antagonists
Nonpharmacologic treatments like transcutaneous electrical nerve stimulation and mirror therapy are part of pain management strategies for PLP, with mirror therapy proving to be particularly effective.
Emerging technologies, such as the DARPA HAPTIX program, are exploring the use of the peripheral nervous system to enhance prosthetic limb control and restore sensation.
Future Directions: Research and Policy Implications
Observing trends in major lower extremity amputation rates is of paramount importance for guiding future research and shaping policy implications. The rates of lower extremity amputations among US Medicare recipients decreased by 40% from 1996 through 2011, but an uptrend has been observed from 2010 through 2015, indicating a changing dynamic of limb loss and lower extremity amputation over the years.
Further research is needed to understand rehabilitation outcomes for different demographics and address gaps in research. There is a recognized gap in research on rehabilitation outcomes for the oldest demographic of lower limb amputees, which may impact the effectiveness and appropriateness of rehabilitation programs.
Frequently Asked Questions
How many people Cannot afford prosthetics?
About 10% of amputees cannot afford a prosthesis due to financial difficulties. This makes it challenging for them to obtain the necessary support.
What is the most common amputated limb?
The most common amputated limb is below-knee, representing 71% of dysvascular amputations. This type of amputation is expected to increase by 47% from 1995-2020.
How many people have no arms or legs?
Close to 2 million people in the US are living with limb loss due to various causes such as vascular disease, trauma, and cancer.
What do you call someone with both legs amputated?
You would call someone with both legs amputated a bilateral amputee. This term is used to describe a person who is missing or has had amputated both legs (or both arms).
What is the most amputated body part?
The most amputated body part is the lower limb, with 90% of all amputations relating to lower limbs. In the United States, amputation of the leg, either above or below the knee, is the most common amputation surgery.